Prions and Alzheimer's Disease
Proteins are absolutely fundamental and essential to life - not least that of humans. Yet when polypeptides misfold - generating "prions" - the consequences can be devastating, and raise numerous questions and concerns.
Legacy articles aren't reviewed and may be incorrectly formatted.
Prions and Alzheimer's Disease
Elliot Dudko
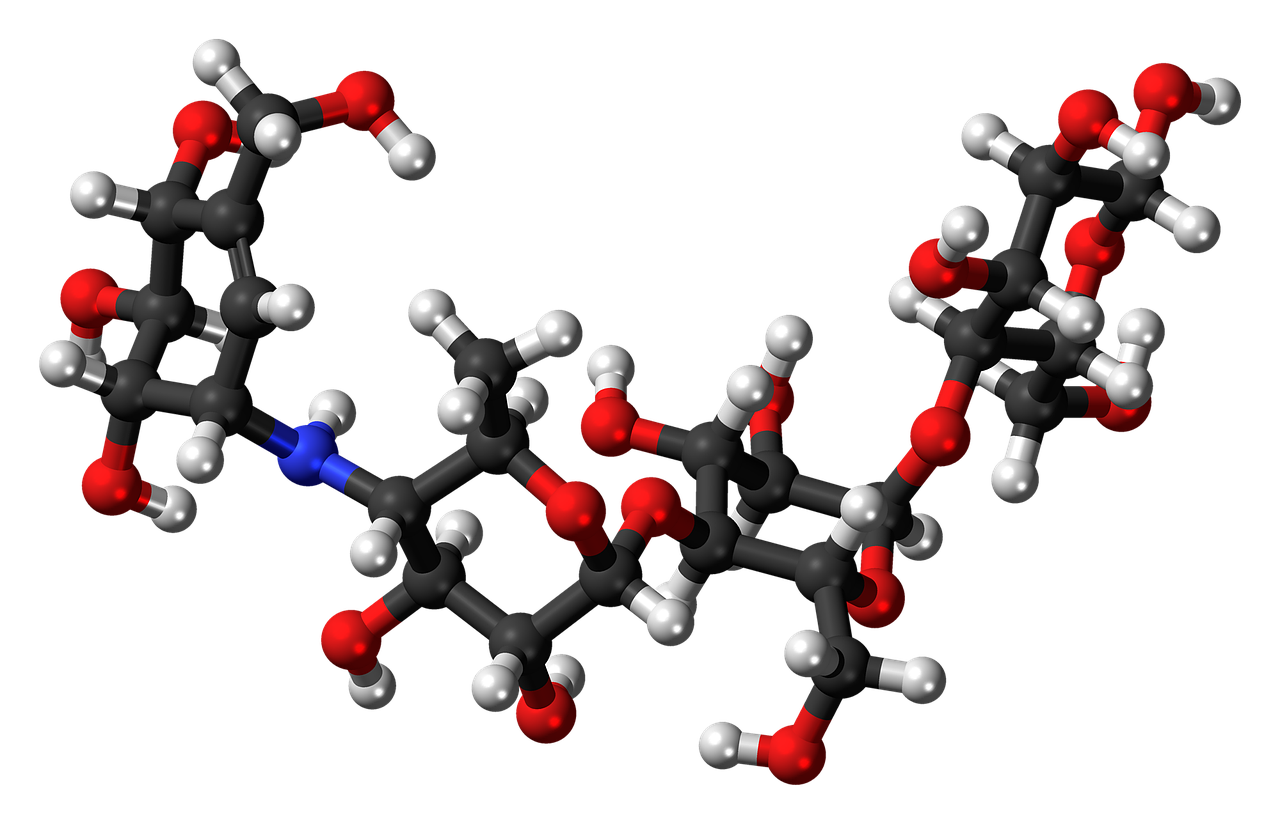
Prions are misfolded versions of a protein. They can spread like an infection by forcing normal copies of that protein into the same self-propagating, misfolded shape. Central to the prion pathogenesis is the conversion of a host encoded protein into a partially protease resistant isoform, meaning that prions cannot be broken down by enzymes, unlike other proteins. This is significant as in close proximity, these isoforms clump together and accumulate in the brain, resulting in the spongiform degeneration of neurones. The ‘protein only hypothesis’ was first established after recognising the ability of transmission to be affected both naturally and experimentally by the disease associated prion protein in the absence of nucleic acid; this was the first time a disease had been shown to infect people not by an infestation of an organism such as a bacterium or virus, but through an infectious protein in 1997.
In an interview, the Colorado State University’s Prion Research Centre explained that “prions are distorted versions of normal proteins found in human and animal brain and other tissue, and technically speaking, proteins shouldn’t be able to infect other proteins - they’re not alive”. Prions are non-living organisms, and, as such, they don’t contain DNA. Yet, they can survive being treated with disinfectants, being boiled, and can still infect other brains years after having initially being transferred. So, just how do these normal proteins misfold into prions, and what causes them to do so?
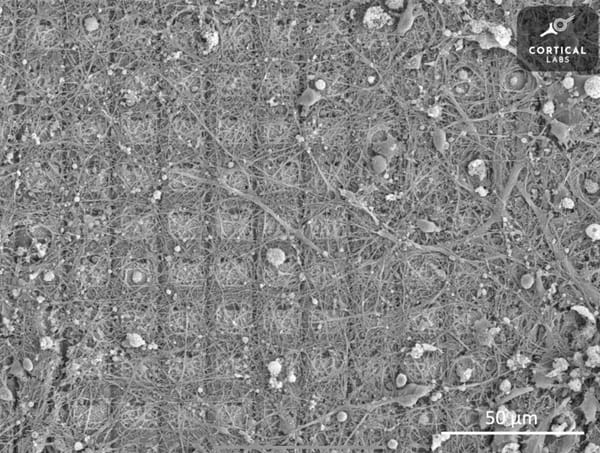
A number of advances in recent years has resulted in the recognition that two proteins central to the pathology of Alzheimer’s disease act as prions; using novel laboratory tests, the researchers were able to detect and measure specific, self-propagating prion forms of the proteins amyloid beta (Aß) and tau in the post mortem brain tissue of 75 Alzheimer’s patients. Furthermore, in a striking finding, it was noted that higher levels of these prions in human brain samples were strongly associated with early onset forms of the disease and a younger age of death. Alzheimer’s disease is currently defined based on the presence of toxic protein aggregations in the brain known as amyloid plaques and tau tangles, which result in the aforementioned spongiform degeneration of neurones. However, although attempts to treat the disease have so far been unsuccessful, new evidence suggests that active Aß and tau prions could be driving the disease. Previously, Alzheimer’s research has been stuck looking at collateral damage in the form of misfolded, dead proteins that form plaques and tangles. Now, it turns out that it is the prions’ activity that correlates to disease, rather than the amount of plaques and tangles at the time of the autopsy. Protein chemist Dr William DeGrado says: ‘if we are going to succeed in developing effective therapies and diagnostics, we need to target the active prion forms, rather than the large amount of protein plaques and tangles’.
Possibly the most notable finding of this new study is the discovery that the self-propagating prions of tau and Aß are most infectious in the brains of Alzheimer’s patients who died at a young age from inherited, genetically driven forms of the disease, but are much less prevalent in patients who died at an older age. In particular, when compared to measurements of overall tau buildup (which is known to increase with age), researchers found a surprising exponential decline in the corresponding abundance of this specific prion form with age. Relative to overall tau levels, the quantity of tau prions in the brain of a patient who died at age 40 were on average 32 times that in a patient who died aged 90.
The research raises a number of questions that will need to be addressed by future studies, including whether differences in prion infectivity could explain the long standing mystery of why Alzheimer’s progresses at such different rates in different patients. Other questions resulting from the research include whether higher prion levels in brain samples from younger patients are linked to the early onset of the disease or how quickly it progressed, and whether lower prion levels in older brains reflect less “infective” prion variants or instead some ability of these patients’ brains to break down and destroy misfolded proteins. Many promising Alzheimer’s therapies have failed in clinical trials, which suggests that scientists have possibly been targeting the wrong proteins. However, at the same time, they may have just not been designing drugs against the distinctive prion forms of these proteins that actually engender disease. Now that scientists have the ability to effectively measure the prion forms of Aß and tau, there is hope that we will be able to develop drugs to prevent these prions from forming or spreading, or even help the brain break them down before any damage is caused.