Lung Conditions and Liquid Ventilation
Humans have lungs adapted to inhale air and use the oxygen in that air which have served vertebrates since around 400Ma. Using liquid for ventilation in lungs would therefore seem absurd. Indeed, in normal healthy lungs, liquid breathing as one would expect worsens gas exchange. However, in cases of
Legacy articles aren't reviewed and may be incorrectly formatted.
Lung Conditions and Liquid Ventilation
Ned van Steenis (JDM)
If I were to describe someone as having liquid-filled lungs, you would probably envisage a person drowning or suffering from pulmonary oedema. After all, humans have lungs adapted to inhale air and use the oxygen in that air which have served vertebrates since around 400Ma.1 Using liquid for ventilation in lungs would therefore seem absurd. Indeed, in normal healthy lungs, liquid breathing as one would expect worsens gas exchange. However, in cases of lung injury, so-called ‘liquid breathing’ works in such a way as to be of substantial medical significance.
In the 1960s, work intended to increase the escape depth of submarines2 found that in hyperbaric conditions, salt solutions could become saturated with oxygen.3 Unfortunately, the pressure of these hyperbaric conditions was too much for vertebrates to withstand whilst the saline solutions became toxic due to the accumulation of CO2. Silicone oils were tested but CO2 accumulated in them as well.4 It was in 1969 that perfluorocarbons (PFCs) were discovered to be suitable for submarines, O2 and CO2 both being very soluble in them.5
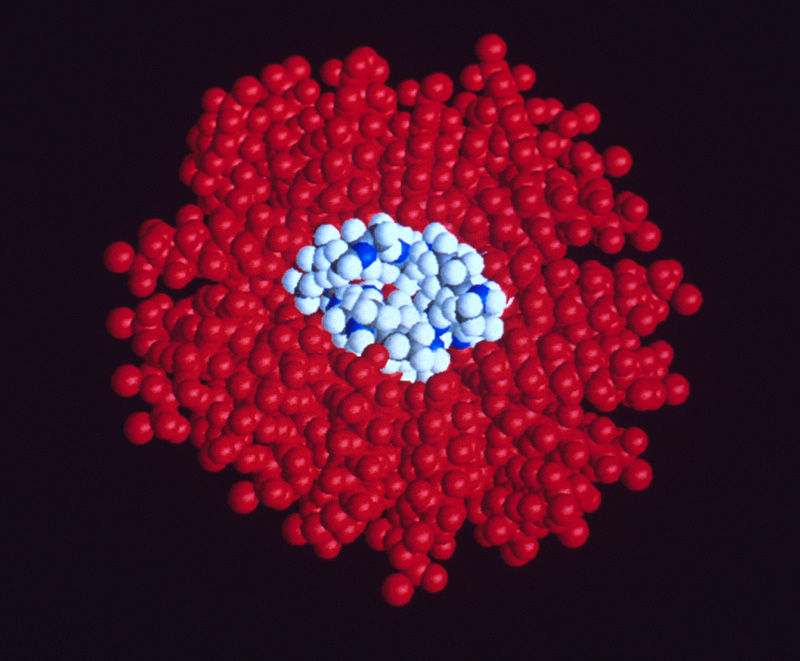
Perfluorocarbons already have other current medical uses in cancer treatment and imaging.6 Usefully, they are inert and are not metabolised by the liver and kidneys7, making them suitable for liquid breathing. They have a higher density than most body fluids, which is important for ensuring that they get into the deepest parts of the lungs where the most atelectasis (incomplete inflation or collapse of the lung) occurs.8 They also have low intermolecular forces reducing their surface tension.9 Most importantly for liquid breathing, at room temperature and pressure they dissolve large quantities of O2 and CO2. 10
There is another important aspect of pressure in liquid breathing. The lining of alveoli has a thin film of water at the air-liquid interface which experiences surface tension. As the water molecules try to minimise their surface area, were there to not be any external forces - in this case the large pressure from inhaled air - the alveoli would collapse. Pulmonary surfactants already in our lungs help to reduce surface tension11, but when the pulmonary surfactant system has been damaged, liquid breathing serves as an excellent treatment: the pressure needed to expand a lung filled with liquid is three times less than that needed to expand a lung filled with air.12
Furthermore, PFCs are helpful in cases of acute lung injury. Acute lung injury is characterised by severe inflammation, causing several issues such as permeability oedema, pulmonary hypertension, and reduced pulmonary compliance as a result of loss or damage to the surfactant system which all result in atelectasis.13 By reopening collapsed lung regions, PFCs improve pulmonary compliance and thus allow alveoli in the affected region to function again. Moreover, PFCs have a mildly anti-inflammatory property, which further aids their efficacy in the treatment. These two properties of PFCs also help in treating Acute Respiratory Distress Syndrome (ARDS), a condition characterised by bodily fluids leaking into the lungs, simply by reducing interfacial tension.14
Liquid breathing treatment is a technological headache. Originally, simple immersion techniques were tested: although this worked, owing to the highly viscous nature of the PFC ‘liquid fatigue’ would render longer liquid breathing unviable. A gravity-assisted approach was also tested with oxygenated PFCs suspended above the vertebrate and allowed to drain into the animal’s lungs with alternating cycles of input and emptying able to supply O2 and remove CO2 from the PFC. However, the PFCs could not be reused making this highly expensive.15 Thus, the PFC is now taken in via an endotracheal tube by which the lungs can be suffused with the PFC without disruption of normal gas ventilation.16 Both total and partial liquid ventilation techniques exist. In total liquid breathing, as one might imagine, the lungs are entirely suffused with a PFC. In partial liquid ventilation, the lungs are filled with a volume of PFC equivalent to its functional residual capacity (the volume remaining in the lungs after a normal exhalation).17 A liquid ventilator is used, achieving optimal carbon dioxide clearance at a rate of 4-5 breaths per minute.18 Partial liquid ventilation appears to achieve more even distribution in the lungs than in total liquid breathing. To be economically viable, the PFC must then be reclaimed and reused.19
Despite all this impressive technology, there are many significant issues. Pneumothorax, where air or gas enters the pleural cavity thus causing lung collapse, has been observed in some trials of PFCs.20 This may be due to insufficient positive pressure in the non-PFC-filled alveoli at the end of exhalation, causing them to collapse.21 Lactic acidosis - where body fluids contain too much acid - has also been recorded, perhaps due to reduced regional blood flow.22 PFCs are taken up by the reticuloendothelial system, a system of phagocytes responsible for removing foreign particles from the body. However, traces of PFC after one hour of exposure have been found three years later.23 There seems to be no inflammatory response to these inert chemicals, but caution should be exercised if any agent remains in the body for such an unexpectedly long time.24
Liquid breathing is remarkable. There is much more to be seen. For instance, Perflubron, C8F17Br, looks to have promising properties for future liquid breathing. And although PFCs were discovered to be suitable around 50 years ago, more effective substances with less side effects need to be looked for. For now, liquid breathing remains a useful oddity.
1. Lung Evolution in Vertebrates and the Water-to-land Transition, Camilla Capella et al. (Elife, 2022) - https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjxjIbLjfSEAxUdgv0HHb4pDL4QFnoECBEQAw&url=https%3A%2F%2Fpubmed.ncbi.nlm.nih.gov%2F35880746%2F%23%3A~%3Atext%3DA%2520crucial%2520evolutionary%2520change%2520in%2Cincluding%2520the%2520acquisition%2520of%2520lungs.&usg=AOvVaw3HctLQuTQgJmIfuyvbhNAJ&opi=89978449 or https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9323002/.
2. Liquid Ventilation, K.P. Kelly, U. Kaisers, and T. Busch (British Journal of Anaesthesia, Vol. 91 Issue 1, July 2003) - https://academic.oup.com/bja/article/91/1/143/276179#.
3. Liquid Breathing, University of Bristol: https://www.chm.bris.ac.uk/webprojects2002/shorrock/3-%20%20Liquid_breathing.htm#:~:text=This%20concept%20originated%20in%20the,build%20up%20of%20carbon%20dioxide.
4. Liquid Ventilation, K.P. Kelly, U. Kaisers, and T. Busch (British Journal of Anaesthesia, Vol. 91 Issue 1, July 2003)
5. Liquid Breathing, University of Bristol
6. Perfluorocarbons: A Perspective of Theranostic Applications and Challenges, Nasrin Kakaei et al. (Frontiers in Bioengineering and Biotechnology, 2023) - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10436007/.
7. Liquid Ventilation, Rajini Kausalya and Qutaiba A. Tawfic (Oman Medical Journal, Vol. 26, Issue 1, January 2011) - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3191624/.
8. One can compare: Perfluorocarbons: A Perspective of Theranostic Applications and Challenges, Nasrin Kakaei et al. with https://itis.swiss/virtual-population/tissue-properties/database/density/.
9. Liquid Ventilation, K.P. Kelly, U. Kaisers, and T. Busch (British Journal of Anaesthesia, Vol. 91 Issue 1, July 2003)
10. Liquid Breathing, University of Bristol
11. Genomic Determinants of Interstitial Lung Disease, Paul W. Noble and Mark P. Steele (Genomic and Personalised Medicine, Vol I & II, 2009) - https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/pulmonary-surfactant
12. Ibid
13. Acute Lung Injury: Disease Modelling and the Therpeutic Potential of Cells, Norashikin Zakaria et al. (Advances in Experimental Medicine and Biology, Vol. 1298) – https://link.springer.com/chapter/10.1007/5584_2020_538 and Ibid.
14. Liquid Ventilation, K.P. Kelly, U. Kaisers, and T. Busch (British Journal of Anaesthesia, Vol. 91 Issue 1, July 2003)
15. Special Ventilatory Techniques and Modalities II, Alan R.Spritzer et al. (Assisted Ventilation of the Neonate, Edition 4, 2003) - https://www.sciencedirect.com/topics/medicine-and-dentistry/liquid-breathing.
16. Liquid Ventilation, Rajini Kausalya and Qutaiba A. Tawfic (Oman Medical Journal, Vol. 26, Issue 1, January 2011)
17. Partial Liquid Ventilation for Preventing Death and Morbidity in Adults with Acute Lung Injury and Acute Respiratory Distress Syndrome, M.W. Davies and J.F. Fraser (Cochrane Database of Systematic Reviews, Oct. 18 2004). See revised version I used: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6516802/
18. Ibid
19. Special Ventilatory Techniques and Modalities II, Alan R.Spritzer et al. (Assisted Ventilation of the Neonate, Edition 4, 2003)
20. Liquid Ventilation in Adults, Children, and Full-term Neonates, R.B. Hirschl et al. (Lancet, November 4th 1995) - https://pubmed.ncbi.nlm.nih.gov/7475663/.
21. Liquid Ventilation, K.P. Kelly, U. Kaisers, and T. Busch (British Journal of Anaesthesia, Vol. 91 Issue 1, July 2003)
22. Ibid
23. Liquid Ventilation, Rajini Kausalya and Qutaiba A. Tawfic (Oman Medical Journal, Vol. 26, Issue 1, January 2011) and Ibid
24. Ibid and Ibid